Coronary Artery Disease
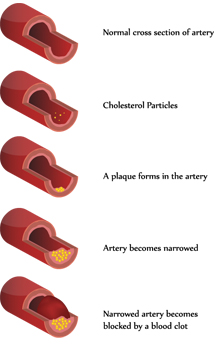
The heart is a muscular organ that pumps blood to the body. Oxygen and nutrients that are required to fuel the pump are carried to the heart in the coronary arteries. The most common cause of coronary artery narrowing is atherosclerosis where fatty deposits (plaques) build up within the coronary arteries.
Major risk factors for developing coronary artery disease include:
- Raised Cholesterol
- High Blood Pressure
- Diabetes
- Cigarette Smoking
- Family History of Coronary Artery Disease
As the arteries become narrowed, blood flow to the heart may be reduced during times of increased need (exercise, emotional stress). The imbalance between the supply and demand of oxygen can cause central chest discomfort. This pain can also radiate into the jaw and down the arms and be associated with breathlessness, nausea and sweating. This is known as angina. When the blockage is severe enough to completely cut off the supply of oxygen to the heart muscle, a heart attack can result.
Patients may remain stable with no change in the frequency or severity of their angina for several years. This is known as stable angina.
In other cases, plaques within artery may develop a slight crack which stimulates the production of blood clots that try to seal off the crack. The clot also gets into the crack and causes it to rise and further obstruct the middle of the artery. The sudden increase in the obstruction caused by the raised ruptured plaque and associated clot can transform a mild blockage into a critical one within a matter of hours. The decrease in blood flow to the heart muscle is severely reduced and the patient begins to have severe and prolonged chest pain that occurs at rest and may even awaken him or her from sleep. This is known as unstable angina.
However, the clot may continue to grow which can completely block the artery and cut off blood flow to the part of the heart muscle that it supplies. Without oxygen and nutrients, the patient suffers a heart attack and the involved heart muscle can get permanently damaged. There are several forms of treatment that can restore blood flow to the artery but this needs to be carried out at as an emergency in hospital.
Hypertension
(High Blood Pressure)
High blood pressure is a major risk factor for developing heart disease. Patients with high blood pressure usually have no symptoms, so the only way to know if you have high blood pressure is to have yours measured.If your blood pressure readings are consistently above 140/85 mmHg you probably have hypertension. This higher pressure puts extra strain on your heart and blood vessels and over time this increases your risk of developing coronary artery disease, kidney disease, stroke and some forms of dementia.
Many things can affect your blood pressure through the day, so your doctor will take a number of blood pressure readings to see that it stays high over time. For most people there is no single cause for their high blood pressure but you are at increased risk if you eat too much salt, are overweight or drink too much alcohol and don't take enough physical exercise. Some cases of hypertension are related to other medical conditions.
Heart Failure
Heart failure is a serious medical condition where the heart is unable to pump enough blood around the body to fulfill all the body's requirements. Patients typically present with a combination of breathlessness and fatigue and this may be associated with swelling of the ankles or the abdomen. Initially patients may only be breathless with significant exercise but as the condition progresses breathlessness may occur with only mid exertion and may be more noticeable when lying down. Patients may start to sleep with more pillows our wake up breathless.
Heart failure is a common condition which affects 1-2% of the UK population and becomes more common as patients grow older. The average age of a heart failure patient in the UK is 76 years but it can affect people of all ages. Heart failure is commonly due to a heart muscle weakness caused by coronary artery disease. Valve disease (a leaking or narrowed heart valve) high blood pressure or inherited heart muscle problems (cardiomyopathy) can also lead to heart failure.
Whilst heart failure is a very serious condition, many treatment options are available including a variety of medications which have been shown to improve symptoms and make patients live longer. Certain patients will also benefit from specialised pacemakers (biventricular pacemaker or cardiac resynchronisation therapy) or implantable defibrillators. Patients often benefit from frequent careful monitoring and gradual changes in medications. With modern therapies, most patients can lead independent fulfilling lives.
Valvular Heart Disease
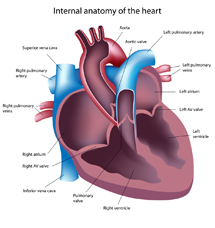
The heart pumps blood to your body and the lungs. It has four chambers that are separated by valves (mitral and tricuspid valve) which ensures blood flows around the heart in the right direction. The two large blood vessels that leave the heart also have valves (aortic and pulmonary valves) to prevent blood flowing back into the heart after it has contracted.
The main causes of heart valve disease in the UK are:
- Congenital Heart Disease
- Damage to the heart valves following a heart attack.
- Cardiomyopathy
- Getting Older
- Infection (Endocarditis)
Damaged valves can affect blood flow in two ways. The valve can become narrowed and reduce blood flow (valve stenosis) or become leaky allowing blood to flow in the wrong direction(valve regurgitation). Both of these will mean that the heart has to work harder to pump blood in the right direction. Initially there may be no symptoms but over time you may experience breathlessness, fatigue and develop swelling of the ankles and in some cases palpitations, dizzy spells and even collapse.
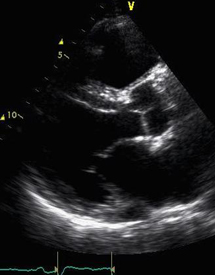
Valvular heart disease results in a murmur which can be detected when a doctor listens to the heart although murmurs can occur in normal hearts as well. The most common test to look at whether there is significant valve disease is an echocardiogram which is similar to an ultrasound scan that is used to look at babies before they are born. The treatment for valvular heart disease depends on the type of valve disease and the effects that it has on your heart.
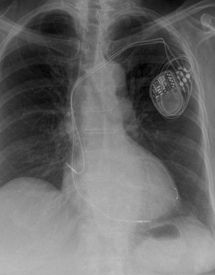
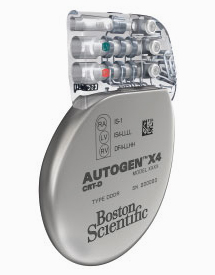
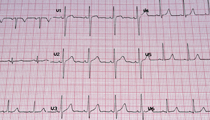
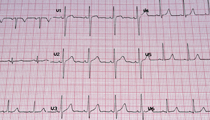
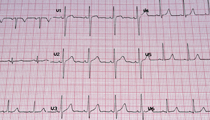
Pacemakers
Pacemakers are most commonly required for patients with a history of collapse or dizzy spells, when ECG monitoring shows that this is due to a slow heart rate. A pacemaker comprises of two main components, the "pacemaker box" which contains a battery and electrical circuit, and the pacing leads (usually one or two leads are required) which are passed along a blood vessel to the heart. The wires can sense when the heart beats normally and if the heart beats too slowly they can produce an electrical impulse to stimulate the heart. The pacemaker box is usually sited under the skin on the upper chest below the collar bone. The procedure is performed under local anaesthesia with sedation if needed. Patients usually need to stay one night in hospital.
A new type of pacemaker, known as a biventricular pacemaker or cardiac resynchronisation therapy is available for certain patients with heart failure. This usually requires 3 leads and improves the timing of the heart which usually leads to improved quality of life and has been shown to prolong life. These pacemakers are only suitable for certain individuals.
Another form of specialist pacemaker called an implantable cardiac defibrillator (ICD) can be implanted in patients who have survived a cardiac arrest or in patients who have had ventricular arrhythmias (fast heart rhythms from the bottom chambers of the heart). The lead detects abnormal rhythms and depending on how the device is programmed the ICD can try to rapidly pace the heart to stop the arrhythmia but if that is not effective it will then shock the heart to restore a normal heart rhythm. An ICD can be combined with a biventricular pacemaker (BiV-ICD) in selected patients with severe heart failure to improve symptoms and improve mortality.
Useful Links
- British Cardiac Society
- British Society of Heart Failure
- Heart Rhythm Society
- British Heart Foundation
- Heart Rhythm UK
- Arrhythmia Alliance
- Pumping Marvellous
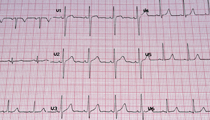
Below is an example of a heart MRI scan.